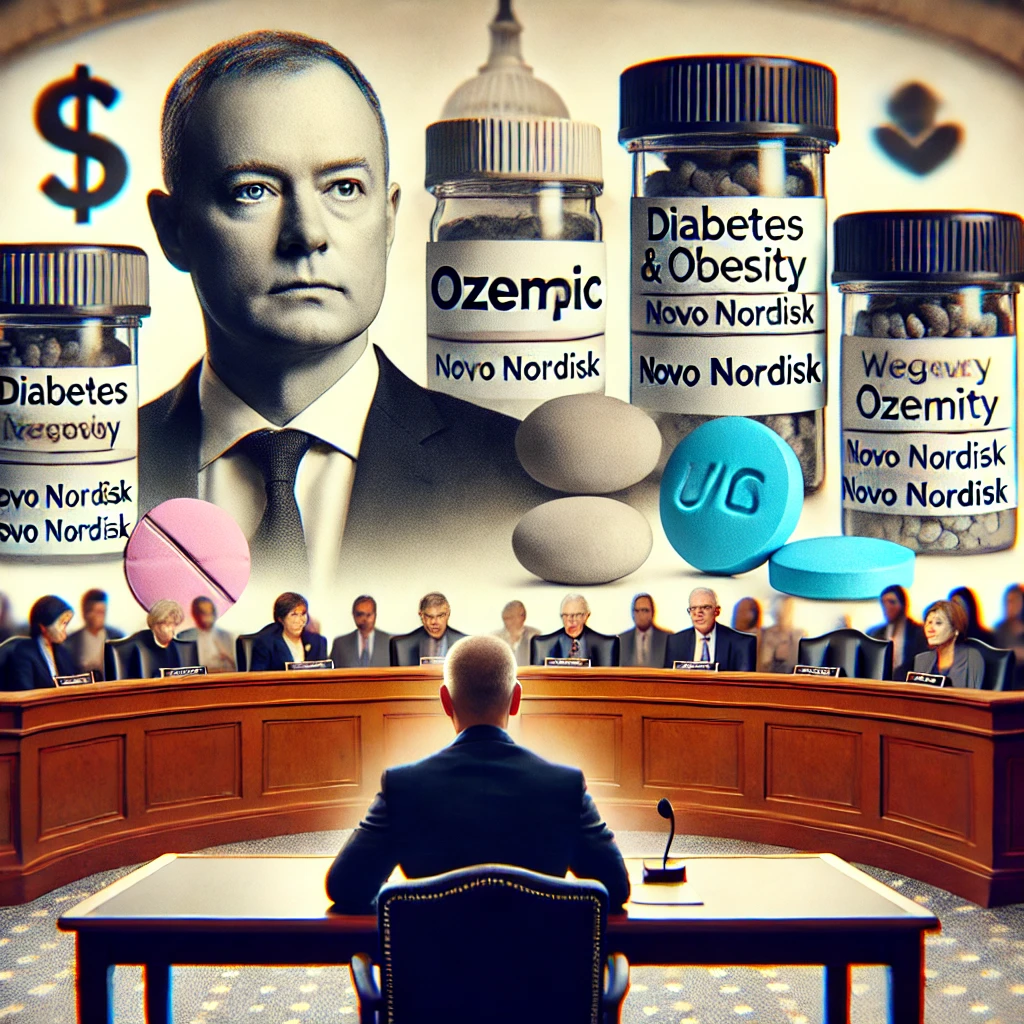
On September 24, 2024, Novo Nordisk’s CEO Lars Fruergaard Jørgensen faced intense scrutiny in a Senate hearing regarding the pricing of Wegovy and Ozempic, blockbuster drugs for obesity and diabetes. The drugs have become essential treatments for many Americans, yet their high U.S. prices—dramatically more expensive than in other countries—have fueled widespread criticism. This issue shines a spotlight on how global pharmaceutical pricing practices and healthcare systems can create inequities, particularly for U.S. consumers.
What the Debate Means for Society
At the heart of the debate is the disproportionate financial burden placed on U.S. patients. For example, Ozempic costs nearly $1,000 per month in the U.S., compared to just $59 in Germany, underscoring the sharp divide in global drug pricing. This inequity raises fundamental questions about healthcare access, fairness, and corporate responsibility. For many patients in the U.S., life-saving drugs are either prohibitively expensive or come with hidden costs in the form of higher insurance premiums, making healthcare access uneven across socio-economic lines.
Senator Bernie Sanders led the charge, framing the issue as a matter of justice, demanding that U.S. citizens receive the same treatment as those in other nations. However, it’s not just the pricing disparities that cause concern; the hearing also unveiled a complicated web of healthcare intermediaries like pharmacy benefit managers (PBMs), who play a crucial role in driving up costs. PBMs, who negotiate rebates with pharmaceutical companies, pocket a large portion of the profits, often at the expense of transparency and patient care.
This debate is not just about drug prices, but about the very structure of the U.S. healthcare system, where corporate profit margins, patient affordability, and pharmaceutical innovation collide. Companies like Novo Nordisk argue that they need revenue to fund research and development, warning that aggressive price cuts could stifle innovation. Lawmakers like Senator Bill Cassidy expressed concern over this delicate balance between making medications affordable and ensuring the continued development of life-saving drugs.
A Larger Systemic Problem
Beyond Novo Nordisk, this debate signals a larger issue within global pharmaceutical practices. The U.S. system is unique in how it involves numerous intermediaries, from insurers to PBMs, which contribute to higher out-of-pocket costs for consumers. Critics argue that these entities introduce inefficiencies that ultimately harm patients.
Globally, other countries negotiate prices directly with pharmaceutical companies, achieving lower prices and ensuring that healthcare remains more affordable. In contrast, U.S. consumers—often with less bargaining power—are left to bear the brunt of higher prices, further widening the gap between those who can afford necessary treatments and those who cannot.
The Path Forward: What Does This Mean for U.S. Patients?
As the demand for price reductions grows, it remains uncertain whether systemic changes will be made in the U.S. healthcare landscape. Companies like Novo Nordisk are open to renegotiating drug prices, but the broader issue of ensuring equitable access to medication while preserving the financial incentives for innovation continues to challenge policymakers.
For society, this ongoing tension reflects deeper ethical questions about healthcare access, corporate responsibility, and how much a person should pay to live a healthy life. Americans, in particular, may find themselves at a crossroads, with lawmakers increasingly pushing for more transparency and equity in drug pricing practices. If successful, such reforms could mark a pivotal shift towards a fairer healthcare system that balances affordability with innovation.
Meta Description
Novo Nordisk’s CEO faces Senate scrutiny over high U.S. drug prices for Wegovy and Ozempic, sparking debates about pharmaceutical pricing inequities and societal impact.
Sources:
- Senate Hearing, September 24, 2024